Immune Signatures in Early Pregnancy: Predicting Outcomes in ART Patients – Reproduction and Fertility
Reproduction and Fertility shared a post on LinkedIn:
“Day 3 of RaFJC – Immune Signatures in Early Pregnancy: Predicting Outcomes in ART Patients
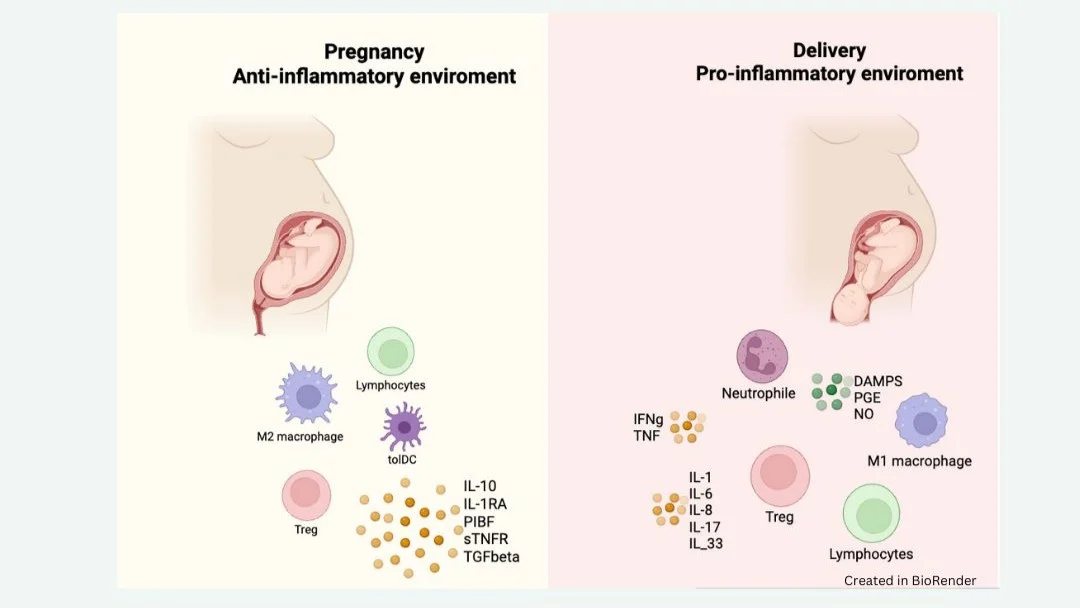
Pregnancy requires a finely tuned immune balance: tolerance of the semi‑allogeneic fetus while maintaining maternal defense against pathogens. Dysregulation of this balance is increasingly recognised as a contributor to implantation failure, recurrent miscarriage, and pregnancy complications.
Recurrent pregnancy loss remains unexplained in up to 40-50% of cases.
Natural killer (NK) cells, T helper subsets, and regulatory T cells (Tregs) are central to maternal immune adaptation.
Identifying early immune markers could allow clinicians to predict pregnancy viability and intervene before complications arise.
Kevin Marron and Conor Harrity performed a prospective pilot study to investigate immune markers in IVF patients at the earliest stage of pregnancy.
Controls:
93 non‑pregnant women analysed in their early follicular phase.
Study group:
65 IVF pregnant women (with unexplained infertility), tested at day 14 post‑frozen embryo transfer after a positive hCG test. The third one of these pregnant women led to a live birth, while 34 ended in miscarriages.
They analysed peripheral blood immunophenotyping by flow cytometry, assessing NK cells, NKT cells, CD4/CD8 T cells, Tregs, and B cells. This design allowed comparison of immune profiles between successful and non‑viable pregnancies at the earliest measurable time point.
This study is the first prospective pilot comparing a comprehensive immunophentyping panel at the exact time of positive hCG, including a differentiation between viable pregnancy and miscarriage cohorts.
What did they find? (image 3)
- B cells (CD19+) and CD57 were increased in all pregnancies, regardless of outcome.
- Treg and CD69 were decreased in pregnancy overall compared to controls (non-pregnant women).
What immune markers were linked to miscarriage? (image 4)
- Reduced pNK CD69+ cells activation during pregnancy, which ended in miscarriage.
- Elevated PNK CD57+ cells during pregnancy, which ended in miscarriage.
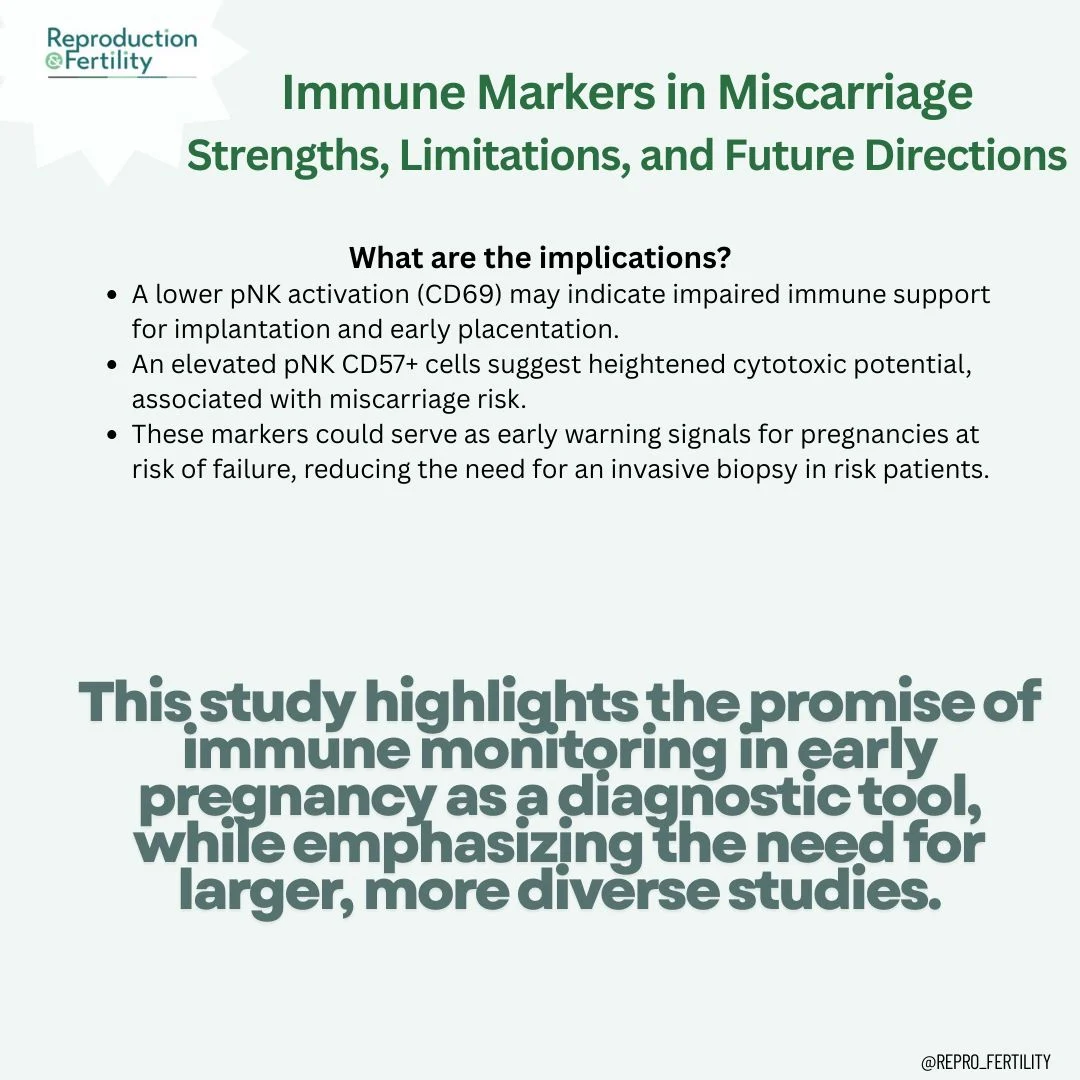
Main interpretations?
- A lower pNK activation (CD69) may indicate impaired immune support for implantation and early placentation.
- An elevated pNK CD57+ cells suggest heightened cytotoxic potential, associated with miscarriage risk.
In conclusion
These markers could serve as early warning signals for pregnancies at risk of failure, reducing the need for an invasive biopsy in high-risk patients. Immune profiling at the time of positive hCG could inform early risk assessment in ART patients.”
Stay updated on all scientific advances in the field of fertility with Fertility News.
-
Oct 11, 2025, 06:44The Global IVF Market Is Set to Reach $65B by 2032 – Meddilink
-
Jan 28, 2026, 16:59Unlocking the Potential of Menstrual Blood in Health Testing – Global Women’s Health Innovation Conclave
-
Jan 28, 2026, 16:57New Insights on Oocyte Yield in Endometriosis and PCOM – RBMO
-
Jan 28, 2026, 16:51Transform Your Expertise with ESHRE eCampus Learning – ESHRE
-
Jan 28, 2026, 16:46Accelerate Your Growth at the AP3G National Meeting – ASRM
-
Jan 28, 2026, 16:43Debojit Saha: Unraveling Chromosomal Errors in Aging Human Eggs
-
Jan 28, 2026, 16:38Silvia Vannuccini: RBMO Highlights Key Insights on Adenomyosis Awareness
-
Jan 28, 2026, 16:32Maximilian Attwood: Challenging Medical Misogyny in Endometriosis Research
-
Jan 28, 2026, 16:29Ioakeim Sapantzoglou: New Perspectives on Fetal Growth Restriction and Genetic Testing
-
Jan 28, 2026, 16:26Enhancing Pre-Eclampsia Prediction with Doppler Indices – ISUOG
